In a previous post, I explained our choice to turn toward chronic disease as our next frontier.
More recently, we have begun a deep dive into Diabetes care. This decision has been influenced by several factors. One is a collaboration with a large telepharmacy chain that is motivated to reshape their value proposition. As they see it, their patients need more from them. And few more urgently than the countless patients with Diabetes – especially those dealing with Type 2 Diabetes.
First – what is it?
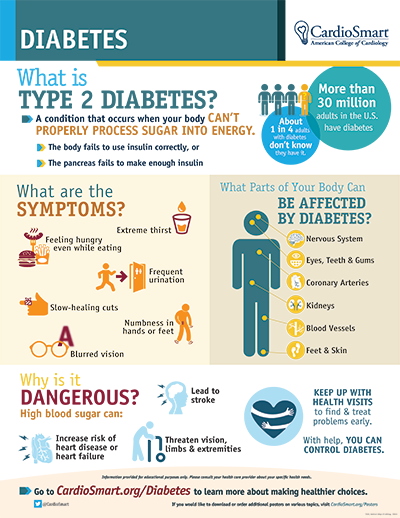
Source: https://www.cardiosmart.org
I thought it wise to then surface some frightening figures that illustrate the scale and growth of the building threat…
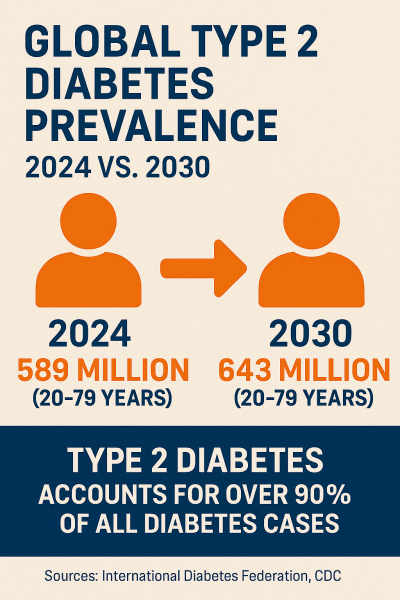
Those are terrible headlines.
But, WHY??? WHY does this persist and continue to worsen??
No matter what data we look at, it’s evident that the situation is going from bad to worse. Here’s a breakdown of why the healthcare industry is falling short in effectively addressing the Type 2 diabetes epidemic in North America and globally:
The System Focuses on Treatment, Not Prevention
- The healthcare model is largely reactive, not proactive.
- Insurance reimbursement and clinic workflows prioritize prescribing medication, not long-term lifestyle coaching, nutrition, or social support.
- Prevention programs often don’t have sustained funding or structure—even though they work.
- And… Only 15% of people with prediabetes in the U.S. are even aware they have it.
Profit Incentives Misalign With Population Health
- Pharmaceutical companies profit from lifelong treatment with insulin, GLP-1s, metformin—not from cures or prevention.
- Hospital systems and device makers benefit financially when patients require complex care and monitoring.
- Junk food and soda industries spend billions in lobbying to maintain their market share, influencing health policy and public perception.
Care is Fragmented & Inequitable
- Many patients—especially in rural, Indigenous, or lower-income communities—face barriers to access: transportation, provider shortages, language gaps.
- Preventive services (nutritionists, diabetes educators, digital health tools) are often uncovered or under-covered by insurance.
- Electronic health records don’t always communicate across providers, limiting coordinated care.
Political Will and Public Health Investment are NOT Rising to the Challenge
- Despite the cost of diabetes (~$400B/year in the U.S., $50B in Canada), public health receives a tiny fraction of overall health spending.
- There is no national diabetes strategy with the scope and power of something like the Cancer Moonshot or HIV/AIDS efforts.
- Prevention doesn’t win elections—acute crisis management does.
Cultural and Systemic Inertia Maintain a Grim Status Quo
- The system is slow to evolve, especially when confronting deeply rooted commercial, cultural, and institutional habits.
- Type 2 diabetes is often seen as a “lifestyle disease”, which leads to stigma and blame, not support and systems change.
- Many clinicians lack time, tools, or incentives to address nutrition, sleep, stress, and social determinants—despite their massive impact.
Health Systems are Not Harnessing Transformative Technology
- While apps and CGMs exist, they are not fully integrated into public health workflows.
- AI and personalized medicine tools are still siloed in clinical trials or corporate wellness programs.
- The vast majority of diabetes-related innovation is profit-driven and excludes underserved populations.
People Are Overwhelmed
- Managing diabetes means constant decisions: food, movement, medication, sleep, stress.
- Without consistent support, education, and culturally sensitive care, people give up or disengage.
- The system rarely funds or supports long-term relationship-based care.
BOTTOM LINE
The failure isn’t just medical—it’s economic, political, and structural.
Solving diabetes at scale requires:
- Shifting incentives toward prevention and early intervention
- Supporting community-based and culturally informed care
- Holding food and pharma industries accountable
- Building a public health infrastructure that sees chronic disease prevention as a national priority
It’s almost exhausting to think about the above. It’s easier to shut it out. Yet, we can’t. It threatens too many of us.
Dave