QiiQ has been around for years now, in grand pursuit of impact. Our unwavering aim is to combine our grasp of clinical workflow’s most thorny challenges with our command of technology’s potent utility as tooling for process therapy.
Along the way, we shifted our central focus from emergency medicine to chronic disease. But it’s much the same in many respects: by applying best practices, we craft solutions that unlock productivity and quality improvement. And while that sounds nice, we’ve come to understand that it’s simply not enough. There are thousands of other tech companies effectively doing the same thing. It’s a wild contest between ambitious and inventive vendors. AI has added accelerant to the frenzy! And yet, despite this feverish competition, the struggles in hospitals and clinics remain largely untouched.
Something more is needed here. And that ain’t an easy matter.
I have a particular take on it. And it’s complicated. Here’s part of it…
Anyone familiar with the healthcare solutions space knows that there are two workflow categories that have recently emerged from obscurity:
- digital intake
- ambient documentation
Both are commoditizing quickly. One could argue they already have.
Along the way, there’s little doubt that improvements have come. Tidy summaries – generated via patient-facing chatbots prior to the exam room encounter – save precious minutes of routine inquiry by physicians during the encounter. Doctors are also largely enthusiastic about the relief of using AI scribes for capturing and summarizing audible dialogue in the exam room. This is non-trivial progress. And we can chalk this one up to AI’s powerful capabilities.
And yet, there is SO MUCH more ground to cover if we hope to encapsulate and impact the patient’s entire odyssey with a brutal disease.
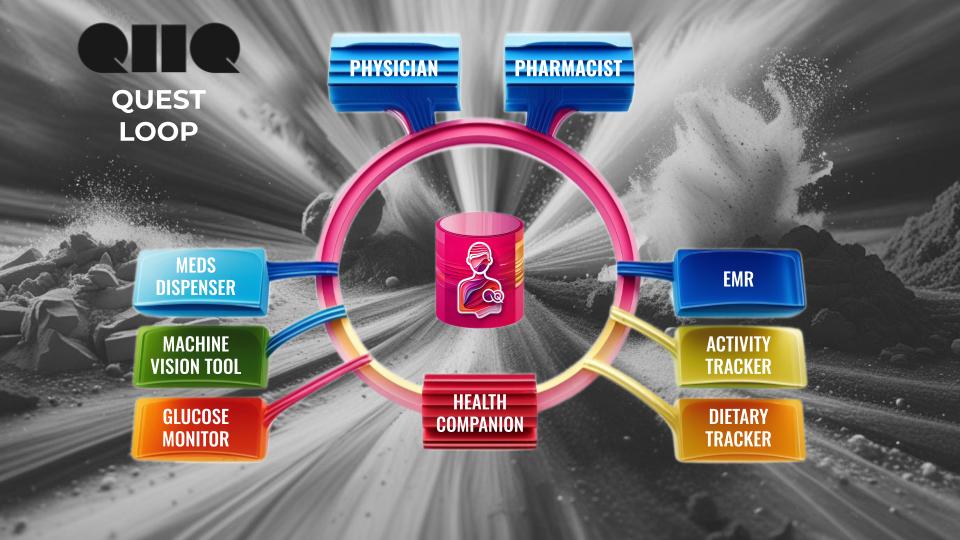
To put this into perspective, I created a simple sketch of data collection through the clinical cycle:
So, where is the gap?
It’s not really accountable to the EMR. I’ll never argue that electronic health record systems deserve awards for usability. They almost all suck. But no-one can claim that the records they contain are data deserts. There’s usually more there than anyone can consume and effectively use. (The challenge is rather to parse these massive information repos for consequential and actionable insights. And there are gazillions worth of R&D dollars pouring into that pursuit).
Thus, as I have been lately proselytizing, some of the most profound gains in clinical impact are to be found in doing a much much better job of capturing and wrangling the data that could be drawn from the patient’s day-to-day challenges in life. Sleep, exercise, medication adherence, diet, and so on…
If we can do that well, and combine that with the other three sources, we have grounds for making a huge difference for the patient, and thus for the massive institutional apparatus dedicated to supporting them.
All 4 of these data touchpoints matter. They all need to contribute interdependently.
With this, we at QiiQ have our calling. And we recognize the deepest challenge lies in patient engagement. As we see it, the winners and losers in the vendor contest are likely to be determined by their ability to capture the patient’s attention, earn their trust, and maintain their loyal adoption by providing significant ongoing value (and fun!?). All it requires that we keep earning their trust by using the data they offer up – to improve their quality of life.
Piece of cake right?
Dave